HCFA-1500 Box 11 - Insured's Policy Group or FECA Number
July 25, 2025
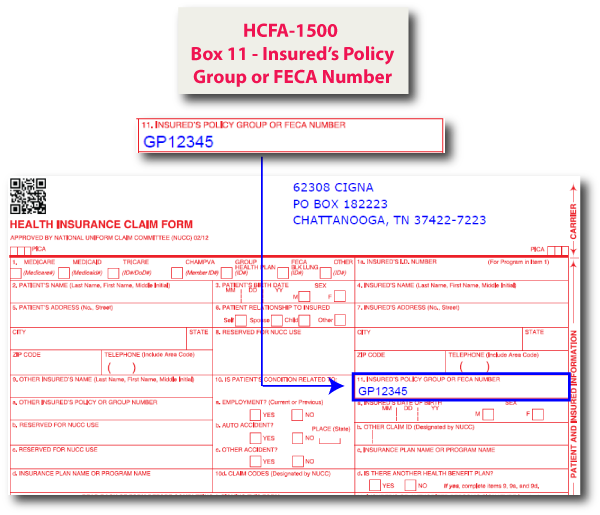
On the HCFA-1500 form, Box 11 is designated for the insured’s policy group or FECA number. This refers to the primary insurance policy number assigned to the patient by the payer, including group numbers or Federal Employees' Compensation Act (FECA) claim numbers.
Completing this box is required for claims involving group health insurance or FECA-related coverage. It ensures the payer can correctly identify the patient's insurance account and apply coverage appropriately.
Tip: Box 11 is required when billing a primary insurance payer. If the patient has no insurance, you may enter “None.” Do not leave this field blank unless directed.
In our example below, we populated Box 11 with the ID 'GP12345'.
So far, we've discussed how the insured’s policy or group number appears on the HCFA-1500 form. In this section, we’ll briefly explore how this information is represented in the X12 837 format.
In the X12 837 transaction, Box 11 maps to the SBR03 data element in the 2000B Subscriber Information Loop, specifically in the SBR (Subscriber Information) segment. SBR03 represents the insured’s group or policy number and is used to report the identifier assigned by the payer for the subscriber’s coverage.
The examples below illustrate how Box 11 maps to the 837 5010 and 4010 formats, specifically within the 2000B loop:
5010 Version:
SBR01 (Payer Responsibility Sequence Number Code): 'P' for Primary
SBR02 (Individual Relationship Code): '18' for Self
SBR03 (Subscriber Group or Policy Number): 'GP12345'
SBR09 (Claim Filing Indicator Code): 'CI' for Commercial Insurance Co.
4010 Version:
SBR01 (Payer Responsibility Sequence Number Code): 'P' for Primary
SBR02 (Individual Relationship Code): '18' for Self
SBR03 (Insured Group or Policy Number): 'GP12345'
SBR09 (Claim Filing Indicator Code): 'CI' for Commercial Insurance Co.
Sample 837P (5010) - 2000B - Subscriber Information
Sample 837P (4010) - 2000B - Subscriber Information
Note: HCFA Box 11 maps to SBR03 in the 2000B loop of the X12 837 for both 4010 and 5010 formats. This field is required when billing a primary insurance payer.
For additional information on the X12 837 standard, please refer to the official implementation guides published by X12.
HCFA-1500 Form Box Locations
- HCFA-1500 Box 0 - Carrier Block
- HCFA-1500 Box 1 - Insurance Type
- HCFA-1500 Box 1a - Insured's ID Number
- HCFA-1500 Box 2 - Patient's Name
- HCFA-1500 Box 3 - Patient's Birth Date and Sex
- HCFA-1500 Box 4 - Insured's Name
- HCFA-1500 Box 5 - Patient's Address
- HCFA-1500 Box 6 - Patient Relationship to Insured
- HCFA-1500 Box 7 - Insured's Address
- HCFA-1500 Box 8 - Reserved For NUCC Use
- HCFA-1500 Box 9 - Other Insured's Name
- HCFA-1500 Box 9a - Other Insured's Policy or Group Number
- HCFA-1500 Box 9b - Reserved For NUCC Use
- HCFA-1500 Box 9c - Reserved For NUCC Use
- HCFA-1500 Box 9d - Insurance Plan Name or Program Name
- HCFA-1500 Box 10 - Is Patient's Condition Related To
- HCFA-1500 Box 10d - Claim Codes
- HCFA-1500 Box 11 - Insured's Policy Group or FECA Number [You are Here]
- HCFA-1500 Box 11a - Insured's Date of Birth and Sex
- HCFA-1500 Box 11b - Other Claim ID
- HCFA-1500 Box 11c - Insurance Plan Name or Program Name
- HCFA-1500 Box 11d - Is There Another Health Plan
- HCFA-1500 Box 12 - Patient's or Authorized Person's Signature
- HCFA-1500 Box 13 - Insured's or Authorized Person's Signature
- HCFA-1500 Box 14 - Date of Current Illness, Injury, Pregnancy (LMP)
- HCFA-1500 Box 15 - Other Date
- HCFA-1500 Box 16 - Dates Patient Unable to Work in Current Occupation
- HCFA-1500 Box 17 - Name of Referring Provider or Other Source
- HCFA-1500 Box 17a - Other ID
- HCFA-1500 Box 17b - NPI
- HCFA-1500 Box 18 - Hospitalization Dates Related to Current Services
- HCFA-1500 Box 19 - Additional Claim Information
- HCFA-1500 Box 20 - Outside Lab Charges
- HCFA-1500 Box 21 - Diagnosis or Nature of Illness or Injury
- HCFA-1500 Box 22 - Resubmission Code and Original Reference Number
- HCFA-1500 Box 23 - Prior Authorization Number
- HCFA-1500 Box 24a - Date(s) of Service
- HCFA-1500 Box 24b - Place of Service
- HCFA-1500 Box 24c - EMG
- HCFA-1500 Box 24d - Procedures, Services, or Supplies
- HCFA-1500 Box 24e - Diagnosis Pointer
- HCFA-1500 Box 24f - Charges
- HCFA-1500 Box 24g - Days or Units
- HCFA-1500 Box 24h - EPSDT/Family Plan
- HCFA-1500 Box 24i - Rendering Provider ID Qualifier
- HCFA-1500 Box 24j - Rendering Provider ID
- HCFA-1500 Box 25 - Federal Tax ID Number
- HCFA-1500 Box 26 - Patient's Account No.
- HCFA-1500 Box 27 - Accept Assignment
- HCFA-1500 Box 28 - Total Charge
- HCFA-1500 Box 29 - Amount Paid
- HCFA-1500 Box 30 - Rsvd for NUCC Use
- HCFA-1500 Box 31 - Signature of Physician or Supplier Including Degrees or Credentials
- HCFA-1500 Box 32 - Service Facility Location Information
- HCFA-1500 Box 32a - NPI
- HCFA-1500 Box 32b - Other ID
- HCFA-1500 Box 33 - Billing Provider Info & Phone No
- HCFA-1500 Box 33a - NPI
- HCFA-1500 Box 33b - Other ID
Grab a sample of the HCFA-1500 claim form here - HCFA 02/12 Claim Form
We hope you found this article helpful! Please reach out to us with questions/feedback.
Disclaimer:
While every effort is made to keep all information up to date and accurate, all content found on Eclaims.com is intended to be a general information resource and is provided "AS IS". The accuracy of the information is in no way guaranteed. Eclaims.com makes no warranty to the accuracy, completeness or reliability of any content available through the website. Eclaims.com assumes no liability whatsoever for any errors or omissions in any content contained on this website. You are responsible for verifying any information before relying on it.